Remote patient monitoring, frequently called RPM, is a type of remote care program that uses connected devices to monitor your patients’ health between office visits.
How RPM Works
Patients use devices like blood pressure monitors, blood glucose monitors, weight scales, and more to measure their vital signs each day, and those results are automatically synced into their provider’s software platform. RPM is typically used to monitor chronic conditions such as hypertension, atrial fibrillation, diabetes, prediabetes, chronic obstructive pulmonary disease (COPD), asthma, and more.
With real-time and additional data on your patient’s health, your practice has the opportunity to provide preventative, patient-centered care that drives proactive interventions, improved outcomes, and higher patient engagement.
Getting Started with RPM
Remote Patient Monitoring (RPM) lets providers stay connected with patients between visits by tracking vitals like blood pressure, glucose, or weight remotely. It’s a proven way to improve chronic care, reduce hospitalizations, and increase engagement.
RPM begins when a clinician at your practice orders it for an eligible patient. After consent is collected, your team provides a connected device, such as a blood pressure monitor or glucometer. An onboarding session, either remote or in-person, helps the patient learn how to use the device and understand the expectations of the program.
Once your patient begins taking readings, that data is securely and automatically transmitted to your RPM platform. Your care team, or a trusted RPM partner, monitors the data, identifies trends, manages care plans, and intervenes when needed.
Common Conditions Monitored with RPM
While RPM can be used to monitor a variety of conditions, it’s most frequently used to support patients with common chronic conditions including:
- Hypertension: The American Heart Association (AHA) recommends that all people with hypertension take their blood pressure every day. For patients with hypertension, RPM helps your practice replace outdated paper logs with daily digital readings. Your team can spot concerning trends early and engage patients with targeted coaching.
- Heart Failure: For patients with heart failure, your team can use RPM to track weight and blood pressure, both of which may reveal signs of fluid retention before a serious exacerbation occurs.
- COPD and Lung Diseases: A pulse oximeter can be used to measure blood oxygen levels and detect early exacerbations of COPD and lung disease.
- Diabetes: RPM with a connected glucometer provides a complete feedback loop for diabetes patients to work with a health coach and understand the impact of their daily activities on their A1C level. A weight scale can also be used to help patients with diabetes or pre-diabetes lose weight and reduce risk of more severe diabetes outcomes.
- Chronic Kidney Disease (CKD): Connected blood pressure monitors and glucometers are frequently used for CKD patients that also have hypertension and/or diabetes. In addition, a weight scale can be used to detect fluid retention, an early sign of worsening kidney failure.
Benefits of RPM
RPM provides real-time visibility on a patient’s health outside of regular office visits, allowing you and your care team to proactively intervene before an adverse event can take place. By using real-time data to prevent critical events, patients benefit from preventative care, and practices are able to provide patient-centered care at a lower cost, delivering both clinical and financial benefits for patients and practices.
Clinical studies demonstrate remote patient monitoring reduces hospital admissions, emergency room visits, and mortality rates. Research also shows that patients in RPM programs can significantly improve the physiological parameters that they are measuring, such as blood pressure or A1C, and avoid emergency room visits and hospital admissions.
For practices, RPM helps providers access real-time patient health data to help patients with chronic conditions and their health each day, rather than relying on office visits alone. In addition, your practice gets reimbursed for the additional preventative care and communications that you provide to patients enrolled in RPM. RPM can also be billed in conjunction with chronic care management (CCM).
RPM programs empower patients to take an active role in improving their health by actively involving them in their health each day. By allowing patients and your monitoring staff to stay connected and communicate more regularly, RPM helps strengthen the patient-provider relationship and support patients more consistently in improving their health.
Insights from the Field: Jared Nelson
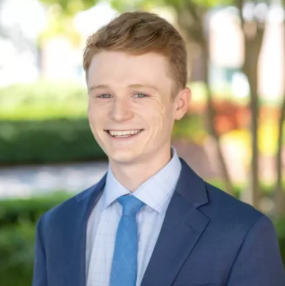
Jared Nelson has spent four years consulting with practices across the country on RPM and chronic care management. In his experience, providers and their teams rely on RPM to:
- Extend care beyond the clinic without hiring additional staff
- Free up clinical teams to spend more time face to face with patients, with confidence that they’ll be alerted to any issues at home
- Strengthen their Chronic Care Management (CCM) program—care managers can easily track vitals from connected devices, helping them triage patients who need attention
Top Questions Clinics Ask About RPM
Jared says he commonly hears the same three concerns from offices regarding RPM:
- “Can our current team handle the day-to-day monitoring? What does that actually involve?”
- “How do we get patients started without burdening our staff, or giving up full control to a third party?”
- “What about the devices? That sounds like a logistical headache.”
Have the Same Questions? Ready to Learn More about RPM?
RPM can improve clinical outcomes, strengthen your relationships with patients, and increase practice reimbursement. If you want to learn more, set up a call with one of our “Jareds” to see if RPM is right for your practice. You can also email us directly at sales@vivocaresolutions.com or call at 888.440.VIVO.
